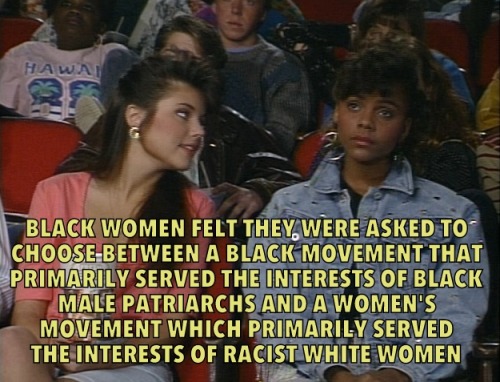
 Some of the potential warning signs of a Covid-19 infection. Patients have reported a variety of symptoms and some, none at all. | Zac Freeland/Vox
Some of the potential warning signs of a Covid-19 infection. Patients have reported a variety of symptoms and some, none at all. | Zac Freeland/Vox
Fever, Covid toes, and a loss of taste: Why are Covid-19 symptoms so weird and varied?
More than six months into the coronavirus pandemic, the list of symptoms caused by the disease Covid-19 is still getting longer.
Beyond the most common symptoms of cough, fever, and shortness of breath, patients have reported other troubling maladies: vomiting, rashes, a loss of taste and smell, muscle aches, and even toe lesions dubbed “Covid toes.”
With more than 16.5 million confirmed cases worldwide, researchers are getting a better handle on the early warning signs of infection and how it plays out throughout the body during the course of the disease. These new insights into symptoms are shedding light on what the virus does to the body, when patients are at highest risk of infecting others, and potential ways to treat it.
And with a larger pool of people recovered from the infection, long-term effects of the illness are also emerging, including symptoms that won’t go away. “Covid-19 can result in prolonged illness, even among young adults without underlying chronic medical conditions,” according to a July 24 Centers for Disease Control and Prevention report. The same report found that one in three symptomatic adults who were surveyed still weren’t fully recovered between two and three weeks after testing positive for Covid-19.
“It is such a unique infection in its ability to cause so much damage in so many different ways, in so many different organ systems,” said Andrew Chan, a professor of immunology and infectious disease at the Harvard T.H. Chan School of Public Health and co-founder of the COVID Symptom Study app. “It’s been very humbling for us as physicians and as a scientific community.”
The growing of list of Covid-19 symptoms, short- and long-term, is yet another example of our evolving understanding of the disease, from how it spreads to how long immunity may last to what treatments may be effective. There is likely much more still to learn about Covid-19 symptoms as scientists gather more data, but here is what they’ve uncovered in recent months about the signs of the disease, how clusters of symptoms can signal more severe complications, and the collateral damage throughout the body.
What the most recent evidence says about Covid-19 symptoms
A recent survey from the CDC identified several symptoms common across the infected. “Among 164 symptomatic COVID-19 patients, nearly all experienced fever, cough, or shortness of breath,” according to a July 17 report from the agency. “However, a wide variety of other symptoms were also reported; chills, myalgia [muscle soreness], headache, fatigue, and the presence of at least one [gastrointestinal] symptom (most commonly diarrhea) were each reported by >50% of patients.”
This aligns with earlier surveys, like one from the World Health Organization back in February, which found conventional symptoms of a respiratory infection were common in Covid-19 patients in China. The most common signs among more than 55,000 confirmed cases were: fever (87.9 percent of confirmed cases), dry cough (67.7 percent), fatigue (38.1 percent), sputum [phlegm] production (33.4 percent), shortness of breath (18.6 percent), sore throat (13.9 percent), and headache (13.6 percent).
But surveys like this from earlier in the pandemic had a harder time detecting milder symptoms. Most of the reports were among patients that were hospitalized or had received medical treatment for Covid-19, meaning they were already experiencing a severe course of the disease. People with less alarming signs were often not detected.
To suss out some of the more subtle symptoms of Covid-19, Harvard’s Chan and his team developed the COVID Symptom Study app, a mobile app that lets users self-report symptoms daily, whether or not they feel sick or have had a test for Covid-19.
/cdn.vox-cdn.com/uploads/chorus_asset/file/20663825/Screen_Shot_2020_07_28_at_6.13.07_PM.png) Radiology
Radiology
The app currently has more than 4 million users in the US alone. By tracking symptoms across large groups of people, Chan and his collaborators have been able to identify emerging Covid-19 hot spots and detect new signals of the virus.
“The symptom that appears to be the strongest predictor of Covid continues to be a loss of taste or smell, and that’s been a thing that’s been continually shown in the data we’re getting in the app,” said Chan. “In particular, the fact that that symptom is relatively uncommon in other viral syndromes, certainly uncommon in seasonal allergies, makes it useful.”
The CDC added a loss of taste and smell to its symptoms guidelines in April, and Chan published his findings in a May 11 paper in the journal Nature Medicine.
Since it’s a more unique symptom to Covid-19 than fever, Chan suggested that screening for taste and smell could serve as a stopgap way to detect infections, especially in places with testing shortages and backlogs. “You can imagine that tests that are able to pick up a loss of smell might be easier to deploy at a large scale, might be more cost-efficient, and could really address some of the shortcomings of our present efforts with respect to testing,” Chan said.
Even more recently, the app has started to pick up signs that skin rashes — raised skin bumps, itchy and red skin, and inflammation on fingers and toes — could be a harbinger of Covid-19 for some. In a recent pre-print paper, a study that has not yet been peer-reviewed, researchers conducted a subsequent survey based on these hints. They found that of 11,546 respondents, 17 percent of people with a confirmed Covid-19 infection reported that a rash was their first symptom. Of the patients reporting rashes, 21 percent said that rashes were their only symptom.
“Even though skin rashes may not be that common in Covid, the fact that they do arise, the fact that they may be a more specific sign, highlight how important it is to really assess their prevalence and how predictive they are,” Chan said.
Other preliminary studies, like one of 204 patients in China, found that more than half of Covid-19 patients experienced gastrointestinal problems like diarrhea, vomiting, and abdominal pain. Some Covid-19 patients reported runny noses. Others experienced feelings of discomfort and malaise. In children, Covid-19 — even previously undetected cases — can spur an inflammatory condition similar to one known as Kawasaki disease. Several elderly people infected with the virus exhibited neurological maladies like confusion and seizures. And patients of all ages have also experienced abnormal blood clotting, causing strokes in otherwise healthy people.
In short, there are a lot of different ways that Covid-19 can show up in a person. But at the same time, an unknown number of people may be infected without showing any outward signs at all. Studies have found the share of asymptomatic patients can comprise anywhere from 18 percent to 40 percent of infected people.
The precise fraction of people infected with Covid-19 who are completely asymptomatic is still being studied, but it’s clear that there are infected people who can spread the virus without coughing or feeling feverish. Even among patients who do show symptoms, some studies have found that they are most infectious just before they start feeling off, rather than when they suffer their worst fevers, rashes, or breathing problems.
That means it’s critical to identify infected people as early as possible and have them isolate from others in order to control the pandemic. And while symptoms can serve as a diagnostic tool in a pinch, robust testing is still needed to identify hidden infections to contain the spread of Covid-19.
Clusters of Covid-19 symptoms can predict more severe complications from the infection
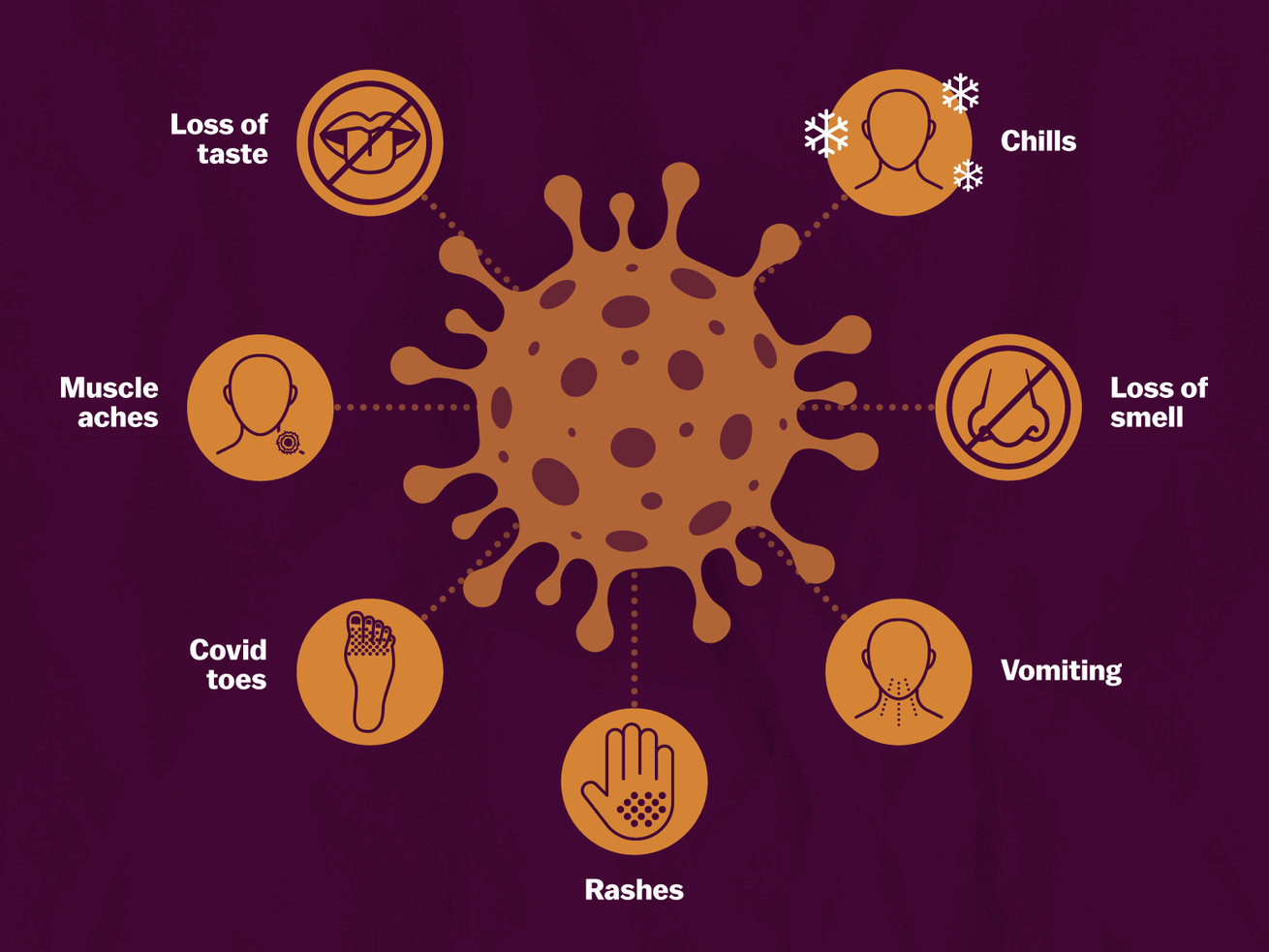
Many Covid-19 symptoms overlap with those of other illnesses, so the patterns of how they emerge together can be a more useful warning sign for the virus than any one symptom alone. In another pre-print paper using data from the tracking app, researchers identified six distinct clusters of symptoms for Covid-19.
These groupings were associated with varying degrees of severity of illness. For instance, among patients experiencing one cluster of symptoms — headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, and muscle pain — 9.9 percent of them ended up needing supplemental oxygen or ventilation.
Meanwhile, patients who experienced the above symptoms, but in addition experienced shortness of breath, diarrhea, and abdominal pain, faced far more severe outcomes. About half of the patients with this second symptom cluster were hospitalized, and 19.8 percent of them required breathing support.
So it’s not just one symptom, but several together that are associated with how the disease progresses. These clusters often emerge in the first five days of the illness, but people who need help breathing often arrive nearly two weeks after they first start showing signs. That means symptom clusters could serve as an early alert, helping health providers anticipate the likelihood of a patient needing to be hospitalized and perhaps prompt earlier treatment.
Being able to identify Covid-19 symptoms matters for preventing spread
When testing is slow or lacking, a cough and fever are often enough for a person to get diagnosed as a Covid-19 patient, with the associated protocols for isolation. And while waiting for a test result, people often have to decide how to isolate from others and take precautions based on what they feel.
After exposure to the virus, it can take two to 14 days for a patient to experience symptoms, if they feel them at all. During that time, these presymptomatic people can spread the virus to other people — especially in the couple of days before they start feeling sick.
Figuring out when key symptoms set in is also important because guidelines for distancing after an infection are often based on when they arise. “For most persons with COVID-19 illness, isolation and precautions can generally be discontinued 10 days after symptom onset and resolution of fever for at least 24 hours, without the use of fever-reducing medications, and with improvement of other symptoms,” according to new CDC guidance based on new information about how long the virus is active and transmissible (emphasis in the original document).
And as the recent findings about symptom clusters show, a specific group of warning signs can signal that a more severe course of the disease is in store in the coming days.
Some symptoms of Covid-19 stem from the immune system’s response
Fever, rashes, and inflammation are often the signs of the immune system’s battle with an infection. But sometimes, the immune system can overreact, causing conditions like cytokine storms where the body overproduces cytokines, signaling molecules that alert cells to an infection. That can cause immune cells to attack otherwise healthy cells, leading to the failure of organs like the liver and kidneys and eventually, death. Even among survivors, this can cause lasting damage.
Still, despite its complexity as a disease, researchers are learning that Covid-19 operates in ways that are distinct from many other infections. Acute respiratory distress syndrome (ARDS) stemming from Covid-19 is a case in point.
ARDS is a condition in some of the most severe Covid-19 cases, causing the lungs to flood with fluid, cutting off oxygen supply to the blood. Patients with ARDS often need to be treated with a ventilator, and are frequently left with severe organ damage.
Nuala Meyer, a critical care lung doctor at the University of Pennsylvania’s Perelman School of Medicine who studies ARDS, typically treats patients suffering with ARDS as the result of the flu. But, she said “the patients we were seeing [with Covid-19] were quite different.”
With flu patients who have ARDS, doctors expect the very worst cases to be among those with asthma, or those who are immunocompromised. Instead, the worst-faring Covid-19 cases were more likely to have heart disease, high blood pressure, diabetes, or obesity. “They generally did not have asthma,” she said. “And some of the patients who were immunocompromised did do really poorly and others did surprisingly well.”
It’s been hard for doctors to predict which Covid-19 patients will fare worse, and develop severe complications like ARDS. But recently, a study from Meyer and her colleagues added new evidence to what’s long been a theory: that it’s not the virus that’s causing the symptoms, but the patient’s own immune system.
In a study of 125 patients, Meyer and colleagues observed three different “immunotypes” or broad patterns of immune response, which may account for the range in severity of disease. It’s currently not clear what leads someone to one immune response or another, but this work, and other work like it, can lead to the detection of biomarkers that indicate people most likely to experience severe disease. Those who had some of the worst outcomes, and spent the most time on a hospital ventilator, were more likely to have dysregulated immune response, Meyers said.
“The fear is that either too persistent an [immune] activation or too robust an activation might contribute to the organ damage that we see,” she said. In Nature, researchers led by Akiko Iwasaki of Yale have noted that many of the most severe Covid-19 symptoms are correlated with an elevated cytokine response, which can lead to damaging inflammation.
The hope is, with a better understanding of the immune response to the SARS-CoV-2 virus, doctors could diagnose patients who are most likely to have this severe reaction, and take steps to prevent the worst reaction from occurring. “That’s where we’d certainly like to go,” Meyer said.
/cdn.vox-cdn.com/uploads/chorus_asset/file/20663815/GettyImages_1227752095.jpg) Marco Di Lauro/Getty Images
Marco Di Lauro/Getty Images
Researchers have already found that drugs that suppress the immune system like dexamethasone can save the lives of the most severely ill Covid-19 patients. But since it tamps down the immune response, it can cause a milder infection to get worse or leave a patient susceptible to another pathogen. That severely limits how useful it can be as a treatment, but it highlights the importance of tuning the immune system to thwart a disease without going any further.
Understanding the immune response to the virus is also critical to making a vaccine for Covid-19, a tool that can ultimately end the pandemic. As knowledge of Covid-19 and immunity improves, researchers expect to gain ground both in fighting the illness and preventing it altogether.
Covid-19 can have ripple effects throughout the body, but the process is still unclear
While Covid-19 is a respiratory infection, it’s become increasingly apparent in recent months that its effects can have cascading consequences throughout the body. Scientists are now piecing together the mechanisms behind these effects in hopes of stopping some of the worst outcomes and to get ahead of long-term problems.
Donald Landry, chair of the department of medicine at Columbia University, co-authored a recent study in the journal Nature Medicine looking at all the ways Covid-19 can impair the body beyond the lungs and airways. The list is long: blood clots, irregular heartbeat, acute kidney injury, gastrointestinal distress, liver damage, high blood sugar, neurologic illnesses, vision problems, and skin complications.
To understand why, it helps to examine how the virus itself works. SARS-CoV-2, the virus behind Covid-19, starts an infection by docking one of its spike proteins with a receptor on a human cell known as ACE2, which is involved in the regulation of blood pressure. So the virus interfering with this mechanism can lead to problems stemming from constricted blood vessels. That interference, plus direct viral damage in blood vessels that have the ACE2 receptor, can cause inflammation and blood clots.
But the virus may be doing something else still unknown that’s causing blood clots. Landry noted that when Covid-19 patients were receiving treatments like ECMO and hemodialysis that involved circulating blood outside the body, the tubing transporting blood in and out of the body also clotted.
“The clotting system itself seems to be revved,” Landry said. “It’s not just inflamed blood vessels; it’s a hyper-coagulable state, so it would seem.”
Those blood clots are dangerous because they can easily choke off tiny blood vessels and impede the blood supply to parts of the body — lungs, kidneys, the liver. However, the damage to those organs can confusingly manifest in other parts of the body. A failing kidney could mean less fluid is removed from the body, leading more fluid to accumulate in the lungs, worsening the respiratory symptoms of Covid-19, according to Landry.
The effects of organ damage can also linger and become permanent, even after the virus is eliminated. If a blood clot blocks a vessel leading to the heart, for example, it can cause the death of a section of heart muscle, a condition known as a myocardial infarction. “You could be surviving the pulmonary part but you could be dying of the cardiac part,” Landry said.
The ACE2 receptors are not just in blood vessels. They can be found in cells in the lungs, so SARS-CoV-2 may be directly causing respiratory symptoms like coughing as it damages those cells. Similarly, heart and kidney cells have this receptor and may be vulnerable to direct attack from the virus, potentially causing some of the observed cardiovascular symptoms.
So there are three potential sources of Covid-19 symptoms: the virus, the immune response to it, and the collateral damage from both. However, sorting out what damage is caused by which mechanism remains a challenge.
“That’s an open question as to what extent is it a primary cytotoxic effect from the virus infection, where it actually damages the cells it’s infecting, versus whether it’s damaging blood vessels,” Landry said. “That whole area needs to be investigated.”
By understanding the mechanisms of Covid-19, doctors can better anticipate the myriad ways it can present and come up with ways to counter its worst effects. But it will take yet more research to build this foundation.
The symptoms of Covid-19 may stick around for a long time
We’re now far enough into the pandemic that millions of people have recovered from Covid-19. While many are no longer contagious, some are finding that the illness has lasting effects on their health.
“For many people, the infection is not a self-limited condition,” Chan said. “Sometimes they’re left with longer-term symptoms that could be quite impairing.”
Already, recovered patients have reported ongoing coughing, trouble concentrating, and muscle weakness. Doctors have also found lesions on the hearts, lungs, and brains of Covid-19 patients that can take a long time to heal and may be permanent in some cases.
“Patients who have had terrible pneumonias or ARDS with Covid-19, are beginning to present now with syndromes of pulmonary fibrosis,” said Landry. “And this is really a grave lesion that can progress to end-stage, requiring lung transplantation.”
Meanwhile, patients with brain damage can suffer lasting speech and mobility issues. Covid-19 survivors with heart damage can have persistent arrhythmias that can make it hard for them to conduct basic tasks. Diminished functions of organs like kidneys could progress and contribute to future health problems.
“There may be many more patients on hemodialysis in the future as a result of the severe damage they suffered to their kidney during the acute Covid-19 [pandemic],” Landry said.
And it’s not just people who fell severely ill who can suffer residual impacts. Even people who had a less severe course of the disease have reported long-lasting symptoms.
Taken together, the early findings about the long-term impacts of Covid-19 show that the world will likely be seeing signs of the illness for years to come — even if the virus were to vanish tomorrow. And in the coming months, even more symptoms and manifestations of the disease may yet emerge.
Support Vox’s explanatory journalism
Every day at Vox, we aim to answer your most important questions and provide you, and our audience around the world, with information that has the power to save lives. Our mission has never been more vital than it is in this moment: to empower you through understanding. Vox’s work is reaching more people than ever, but our distinctive brand of explanatory journalism takes resources — particularly during a pandemic and an economic downturn. Your financial contribution will not constitute a donation, but it will enable our staff to continue to offer free articles, videos, and podcasts at the quality and volume that this moment requires. Please consider making a contribution to Vox today.